Barrett’s Esophagus
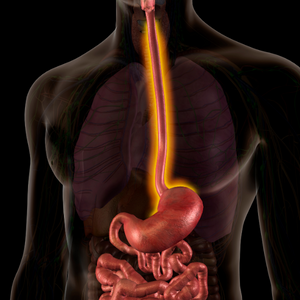
Esophagus is also known as the food pipe or the tube connecting your mouth and stomach. Barrett’s esophagus is a term that refers to replacement of normal lining tissue in the esophagus by tissue similar to small intestinal lining, a process also called intestinal metaplasia.
This change occurs as a complication (estimated at 10-15%) of long-term regurgitation (wash back) of acid and other contents from the stomach into the lower esophagus, a condition also called gastroesophageal reflux disease (GERD). This change in the lining usually causes no symptoms and diagnosis needs endoscopy and biopsy.
Barrett’s esophagus is genetically unstable, especially with continuing inflammation due to acid reflux and can accumulate multiple chromosomal alterations, and eventually progress to dysplasia or esophageal adenocarcinoma. Barrett’s esophagus is therefore associated with a small increased risk of developing esophageal cancer. This risk is approximately 0.5 percent per year (or 1 out of 200).
Dysplasia
Dysplasia refers to presence of abnormal cells within a tissue, which may signify a stage preceding the development of cancer. It appears that Barrett’s esophagus goes through stages of low grade and high grade dysplasia before cancer develops. These changes can only be identified by microscopic examination of Barrett’s tissue. When dysplasia is reported on biopsies, it may lead to more frequent surveillance endoscopies, use of advanced endoscopy techniques to destroy the Barrett’s lining or referral for esophageal surgery. Factors that increase risk of Barrett’s and cancer include acid reflux that doesn’t respond to medications, older age, male sex, white race, increased body fat and smoking.
Follow Up Endoscopy
A diagnosis of Barrett’s esophagus should not be a reason for alarm. It is, however, a reason for periodic surveillance endoscopies. At initial diagnosis and subsequent surveillance endoscopies, biopsies will be evaluated for dysplasia.
FAQs
Barrett’s esophagus is caused by damage to the cells in the lining of the esophagus, typically as a result of chronic acid and bile reflux.
Barrett’s esophagus itself usually does not cause any symptoms, but symptoms of acid reflux, such as heartburn and difficulty swallowing, may be present.
Barrett’s esophagus is usually diagnosed by a biopsy of the lining during an upper endoscopy, a procedure in which a small camera is inserted through the mouth to look at the inside of the esophagus.
Treatment for Barrett’s esophagus typically involves medications to reduce acid reflux and prevent further damage to the esophagus. The most important part of treatment of Barrett’s esophagus involves long term surveillance with repeat endoscopy and biopsies of the lining to look for change in the cells called dysplasia. This change makes it more likely to develop cancer in the future.
The risk of developing esophageal cancer is higher in people with Barrett’s esophagus than in the general population. However, the risk is still relatively low, and most people with Barrett’s esophagus will not develop cancer. This risk is approximately 0.5 percent per year (or 1 out of 200). Regular surveillance with endoscopy is usually recommended to monitor for any changes.
Barrett’s esophagus is typically caused by acid reflux, so preventing acid reflux may help to prevent the development of Barrett’s esophagus. This can include lifestyle changes such as avoiding foods and drinks that cause acid reflux, not eating close to bedtime, and maintaining a healthy weight.
While Barrett’s esophagus cannot be completely cured, it can be treated and managed to prevent the progression to cancer. Treatment options, such as medications and surgery, can help to reduce acid reflux and remove abnormal cells.
Barrett’s esophagus is a chronic condition and typically does not go away on its own. It is important to receive treatment and ongoing surveillance to manage the condition and prevent progression to cancer.
Yes, most people with Barrett’s esophagus are able to live a normal life with the condition. Treatment and lifestyle changes can help to manage symptoms and prevent progression to cancer. It is important to work closely with your doctor to develop an appropriate treatment plan.