Cholangiocarcinoma
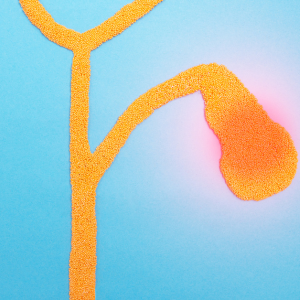
Cholangiocarcinoma is a type of cancer that arises from the bile ducts, which are the tubes that transport bile from the liver to the small intestine. Cholangiocarcinoma can be classified into two main types: intrahepatic cholangiocarcinoma, which starts in the bile ducts within the liver, and extrahepatic cholangiocarcinoma, which starts in the bile ducts outside of the liver. Cholangiocarcinoma is a relatively rare type of cancer, but its incidence has been increasing in recent years.
Risk Factors
- Age: the incidence of cholangiocarcinoma increases with age, with the majority of cases occurring in people over the age of 60.
- Gender: men are slightly more likely to develop cholangiocarcinoma than women.
- Geography: cholangiocarcinoma is more common in certain geographic areas, such as Southeast Asia and parts of Africa, where the prevalence of liver flukes, a type of parasitic infection, is high.
- Medical conditions: people with certain medical conditions such as primary sclerosing cholangitis (PSC) or ulcerative colitis (UC) are at an increased risk of developing cholangiocarcinoma.
Symptoms
The symptoms of cholangiocarcinoma can vary depending on the location and stage of the tumor, but some common symptoms include:
- Jaundice (yellowing of the skin and eyes).
- Itching.
- Abdominal pain, especially in the upper right side.
- Fatigue and weakness.
- Loss of appetite and weight loss.
- Nausea and vomiting.
- Fever and chills.
- Dark urine and pale stools.
Tests
- Laboratory tests: blood tests such as liver function tests, tumor markers like CA19-9, can be used to evaluate the overall health of the liver and to detect the presence of cancer.
- Imaging tests: such as computed tomography (CT) scans, magnetic resonance imaging (MRI) scans, and ultrasound can be used to create detailed images of the liver and bile ducts. These images can help to identify the presence and location of a tumor.
- Endoscopic retrograde cholangiopancreatography (ERCP): this test combines X-ray and endoscopy to examine the bile ducts and pancreas. A small tube is passed through the mouth, down the throat and into the stomach and small intestine. Dye is then injected and X-ray images are taken to visualize the bile ducts and pancreas. This is the best way to obtain a biopsy of the tumor. A biopsy is a procedure in which a small sample of tissue is removed and examined under a microscope to determine if cancer cells are present.
- Endoscopic ultrasound (EUS): this test combines endoscopy and ultrasound to create images of the bile ducts and surrounding structures. An ultrasound probe is passed through the mouth and into the stomach and small intestine. Needle biopsies of the tumor or lymph nodes can be performed with ultrasound guidance.
Treatment
Treatment options for cholangiocarcinoma depend on the stage and location of the tumor, as well as the patient’s overall health. The main treatment options include:
- Surgery: this is the primary treatment for cholangiocarcinoma, and it can be curative if the tumor is caught at an early stage. The type of surgery performed depends on the location of the tumor.
- For tumors located in the bile ducts outside the liver, the surgery is called a bile duct resection. This procedure involves removing the affected portion of the bile duct, along with some surrounding lymph nodes, and reconnecting the remaining healthy portions of the bile duct.
- For tumors located inside the liver, a liver resection may be performed. This procedure involves removing the affected portion of the liver and reconnecting the remaining healthy portions of the liver.
- Radiation therapy: radiation therapy uses high-energy beams to kill cancer cells. It can be used as a primary treatment or as an adjuvant therapy after surgery to reduce the risk of recurrence.
- Chemotherapy: chemotherapy uses drugs to kill cancer cells. It can be used as a primary treatment or as an adjuvant therapy after surgery to reduce the risk of recurrence.
- Some centers offer liver transplantation: depending on the stage of the tumor and overall fitness of the patient.
- Targeted therapy: targeted therapy uses drugs that target specific molecules on the surface of cancer cells, slowing down or stopping their growth.
- Palliation: in advanced cases where the cancer cannot be cured, palliative treatments can be used to improve the patient’s quality of life and to control symptoms such as jaundice and pain.
It’s important to note that the treatment plan is tailored to the individual patient and should be discussed with the oncologist or liver specialist. Additionally, there are some clinical trials that can offer new treatments. It’s important for patients to have a multidisciplinary approach with a team of specialists to provide the best outcome for the patient. The prognosis for cholangiocarcinoma is generally poor, with a five-year survival rate of around 10-15%.
FAQs
The exact cause of cholangiocarcinoma is not known, but certain risk factors have been identified, such as primary sclerosing cholangitis (PSC), a condition that causes inflammation and scarring of the bile ducts, liver fluke infestation, etc.
Symptoms of cholangiocarcinoma can include jaundice (yellowing of the skin and eyes), itching, abdominal pain, weight loss, and fatigue.
Cholangiocarcinoma is diagnosed using a combination of tests, including imaging tests such as CT scans and MRI, endoscopic retrograde cholangiopancreatography (ERCP) and endoscopic ultrasound (EUS), and biopsy.
Treatment options for cholangiocarcinoma depend on the stage and location of the tumor, as well as the patient’s overall health. Treatment options include surgery, radiation therapy, chemotherapy, targeted therapy and palliative treatments.
The prognosis for cholangiocarcinoma is generally poor, with a five-year survival rate of around 10-15%. However, early detection and treatment can improve the chances of survival.
There are some clinical trials available for cholangiocarcinoma, which offer new treatments. It’s important for patients to discuss with their oncologist or liver specialist about the availability of the clinical trials and whether it’s appropriate for their condition.
There is no sure way to prevent cholangiocarcinoma, but reducing risk factors can decrease the chance of developing the disease. Some steps that can be taken include:
- Maintaining a healthy diet and weight.
- Managing underlying medical conditions such as primary sclerosing cholangitis (PSC) and cirrhosis.
- Avoiding alcohol and tobacco.
- Regular check-ups and screenings if you have a family history of cholangiocarcinoma or inherited genetic conditions.
Cholangiocarcinoma can recur after treatment, especially if the cancer has spread to other parts of the body before treatment. Regular follow-up scans and monitoring are important to detect recurrence as early as possible.
In some cases, a liver transplant may be considered as a treatment option for cholangiocarcinoma. The success of transplantation depends on many factors, including the stage of the cancer at the time of transplantation.
Cholangiocarcinoma can spread to other organs such as the liver, lungs, bones, and lymph nodes, which is called metastasis. This occurs when cancer cells break away from the primary tumor and travel through the bloodstream or lymph system to other parts of the body. This is why it’s important to detect and treat the cancer as early as possible to reduce the risk of spread.