Colon Polyp
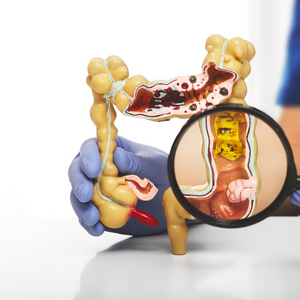
A polyp is an abnormal outgrowth of tissue from the inner lining of the colon which extends into the lumen of organs such as the colon, stomach or small intestine. This occurs occasionally as an anomaly develops in the normal regeneration process of the lining.
Polyps are benign (non-cancerous) growths, but certain types of polyps can transition into cancer. Polyps can be flat or sessile and shaped like a mushroom or pedunculated (with a pedicle or stalk). To prevent polyps with cancer potential (precancerous polyps) from becoming cancerous, they must be removed.
Polyp Appearance
Sessile Polyps
Sessile polyps are flat polyps attached directly by its base to the colon lining without a stalk or a pedicle. These are harder to detect than pedunculated polyps but can be detected by a careful exam and removed safely. They are also more common than previously thought.
Pedunculated Polyps
Pedunculated polyps resemble mushrooms as they attach to the surface of the colon’s mucous membrane by a stalk. They are easier to detect and can be removed in one piece.
Pathology
Adenoma(s)
A vast majority of the polyps called adenomas, begin in the cells of gland forming structures lining the colon. These types of polyps are not cancerous, but they are precancerous (meaning that they can turn into cancers). Adenomas can have several different growth patterns that can be seen under the microscope by the pathologist. There are 2 major growth patterns: tubular and villous. Some adenomas have a mixture of both growth patterns, and are called tubulovillous adenomas.
Serrated Polyps
Serrated polyps have a saw-tooth appearance under the microscope. These types of polyps are not cancerous, but they are precancerous (meaning that they are capable of turning into cancers). Based on the appearance under a microscope, they are further broken down into sessile serrated polyps and traditionally defined serrated adenomas. Sessile serrated polyps larger than 1 cm in diameter and traditionally defined serrated adenomas have a higher risk of progression to cancer needing close follow up.
Hyperplastic Polyps
Hyperplastic polyps are benign and generally not precancerous.
Lymphoid Nodule
These nodules are small, localized collections of lymphoid tissue, usually located in the loose connective tissue beneath the epithelial (covering or lining) membranes. These are not harmful in any way and do not lead to cancer.
Dysplasia
Dysplasia is a term that describes how much your polyp looks like cancer under the microscope. Polyps that are only mildly abnormal (don’t look much like cancer) are said to have low-grade dysplasia. Polyps that are more abnormal and look more like cancer are said to have high-grade dysplasia. As long as your polyp has been completely removed and does not show cancer, you do not need to worry about dysplasia in your polyp. The doctor performing the colonoscopy will have more insight into the issue of complete removal and need for close follow up.
Follow Up Colonoscopy
Having precancerous polyps increases risk of developing cancer of the colon later. Since you had a precancerous polyp, you will need to have another colonoscopy to make sure that all precancerous polyps are detected and removed in a timely fashion. When your next colonoscopy should be scheduled depends on a number of things, such as size and type of polyps as well as on presence of dysplasia. Additionally, when large polyps are removed in a piecemeal fashion, the follow up interval may be shorter than usual.
Polyp Prevention
You can reduce the risk of developing future polyps and colorectal cancer. We recommend adopting healthy habits such as not smoking, maintaining a healthy body weight, being physically active, limiting red and processed meat (such as beef, cold cuts, bacon, and hot dogs), minimizing alcohol intake (or avoiding alcohol altogether), and eating a diet with a lot of fruits and vegetables. It’s not possible to eliminate risk of polyp formation entirely but polyps are easily removed by colonoscopy, which eliminates the risk of cancer in most cases.
FAQs
Colon polyps are growths that develop in the lining of the colon. They can be:
- Benign polyps which can be precancerous or non-precancerous.
- Non-precancerous, which refers to cells or tissue that do not have the potential to turn into cancer.
- Precancerous which refers to abnormal cells or tissue that have the potential to turn into cancer. These cells or tissue have not yet become cancerous, but there is a risk that they could develop into cancer if left untreated.
- Malignant or cancerous polyps.
The exact cause of colon polyps is not known, but certain factors such as age, genetics, and lifestyle choices (such as diet, smoking and lack of exercise) may increase the risk of developing colon polyps.
Colon polyps can be detected during a colonoscopy, a procedure that uses a flexible tube with a camera to visualize the inside of the colon. They can also be detected through stool tests or imaging tests such as CT colonography.
Treatment for colon polyps depends on the type and size of the polyp. Small, benign polyps can be removed during a colonoscopy and no further treatment is required. Most large polyps can be removed as well with special techniques during colonoscopy. Some larger or malignant polyps may require surgery or other treatments such as chemotherapy or radiation therapy.
If a colon polyp is not treated, it may continue to grow and have the potential to develop into colon cancer. This is why it is important to undergo regular colon cancer screening tests and remove all precancerous polyps while they are still benign.
Many colon polyps do not cause any symptoms, but some polyps, especially large ones, can cause symptoms that can include rectal bleeding, changes in bowel habits, abdominal pain or discomfort, and iron deficiency anemia.
A healthy diet and lifestyle, and avoiding smoking and excessive alcohol consumption can also help reduce the risk of developing colon polyps. Regular screenings for colon cancer, such as colonoscopy, can help detect and prevent colon polyps from progressing to cancer.
Benign colon polyps are non-cancerous growths that do not spread to other parts of the body and are unlikely to cause harm. Malignant colon polyps, on the other hand, are cancerous and have the potential to spread to other parts of the body and cause harm.
While most colon polyps are benign, some have the potential to develop into colon cancer over time. This is why it is important to have regular screenings for colon cancer and remove colon polyps while they are still benign.
The frequency of colonoscopy screenings for colon polyps depends on your risk factors and personal history. When your next or follow up colonoscopy should be scheduled depends on a number of things, such as size and type of polyps as well as on presence of dysplasia. Additionally, when large polyps are removed in a piecemeal fashion, the follow up interval may be shorter than usual.
After a colonoscopy to remove a polyp, you may experience some mild discomfort and bloating as the gas used to inflate the colon during the procedure is passed. These symptoms should resolve within a day or two. You may also have a small amount of blood in your stool for a day or two after the procedure. It is important to drink plenty of fluids and follow your doctor’s instructions for care after the procedure.
Yes, Colon polyps can come back after they are removed if the entire polyp is not removed during the colonoscopy. Our Physicians make every effort to ensure that the polyp is removed completely to avoid recurrence of the polyps. It is also possible for new colon polyps to develop after polyps have been removed, particularly if you have had multiple polyps in the past or have other risk factors for developing polyps (such as a family history of colon cancer). This is why it is important to undergo regular colon cancer screening tests as recommended by your doctor to monitor for new polyps.
There is no scientific evidence that natural remedies can prevent or treat colon polyps. However, eating a healthy diet, getting regular exercise, and not smoking can help reduce the risk of developing colon polyps.
A tubular adenoma is a type of precancerous polyp that develops in the colon or rectum. It is called a tubular adenoma because it has a tubular shape and is composed of glandular tissue. Tubular adenomas are considered precancerous because they have the potential to develop into colorectal cancer. They are usually benign (non-cancerous) but a small percentage of them can become malignant over time.
The risk of malignant transformation is related to the size and the histological characteristics of the polyp, the larger and more dysplastic the polyp, the higher the risk of malignancy. Tubular adenomas are usually found during colonoscopy and can be removed during the same procedure.
A tubulovillous polyp is a type of precancerous polyp that develops in the colon or rectum. It is called a tubulovillous polyp because it has both tubular and villous structures. Villous structures are finger-like protrusions of the lining of the colon, while tubular structures are small, tube-like structures. Tubulovillous polyps are considered precancerous because they have the potential to develop into colorectal cancer. They are usually benign (non-cancerous) but a small percentage of them can become malignant over time.
The risk of malignant transformation is related to the size and the histological characteristics of the polyp, the larger and more dysplastic the polyp, the higher the risk of malignancy. Tubulovillous polyps are usually found during colonoscopy and can be removed during the same procedure.
A villous polyp is a type of precancerous polyp that develops in the colon or rectum. It is called a villous polyp because it has finger-like protrusions of the lining of the colon, called villi. These villi can be large and broad or small and delicate, and they give the polyp a hairy appearance. Villous polyps are considered precancerous because they have the potential to develop into colorectal cancer. They are usually benign (non-cancerous) but a small percentage of them can become malignant over time.
The risk of malignant transformation is related to the size and the histological characteristics of the polyp, the larger and more dysplastic the polyp, the higher the risk of malignancy. Villous polyps are usually found during colonoscopy and can be removed during the same procedure.
A sessile serrated polyp (SSP) is a type of precancerous polyp that develops in the colon or rectum. It is called a sessile serrated polyp because it has a flat or slightly raised shape and a serrated or saw-toothed border. SSPs are considered precancerous because they have the potential to develop into colorectal cancer.
Sessile serrated polyps are known to be associated with a higher risk of malignancy than traditional adenomas, and are thought to be responsible for a significant proportion of colorectal cancer cases. They are typically smaller than traditional adenomas and can be harder to detect during a colonoscopy. SSPs can be removed during colonoscopy.
A hyperplastic polyp is a type of benign (non-cancerous) polyp that develops in the colon or rectum. It is called a hyperplastic polyp because it is made up of an abnormal overgrowth of cells in the lining of the colon or rectum. These polyps are typically small, measuring less than 1 cm, and are usually non-cancerous.
Hyperplastic polyps are considered to be less of a concern for colon cancer risk compared to other types of polyps, such as adenomas or sessile serrated polyps. They are usually found during a colonoscopy and can be removed during the same procedure.