Pancreatic Cysts
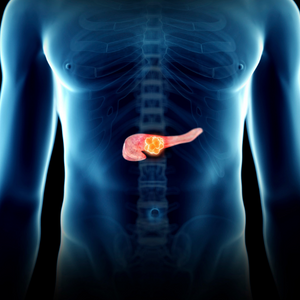
Pancreas cysts are fluid filled sacs arising within or from the pancreas, a large gland that sits behind the stomach. Pancreas gland produces digestive juices, which it delivers to the small intestine via a hollow tube called the pancreas duct. It also makes hormones such as insulin.
Pancreas cysts are most commonly discovered by accident on CT or MRI scan performed for other reasons. Pancreatic cysts are common and are found in over 20% of people over the age of 70 undergoing imaging tests for other reasons. Many pancreatic cysts are small (few millimeters) and benign and produce no symptoms, but some cysts become large (several centimeters) and cause symptoms.
Symptoms
The vast majority of pancreatic cysts are asymptomatic. If pancreatic cysts are large or advanced, symptoms can include:
- Abdominal pain sometimes radiating to the back.
- Nausea with or without vomiting.
- Abdominal bloating.
- A mass or lump you can feel in your upper abdomen.
- Weight loss.
- Jaundice (yellowing of the skin and eyes with darkening of the urine).
Significance
The potential of some pancreatic cysts to progress to pancreatic cancer, is the reason for their significance. Pancreas cysts can be divided into two broad categories based on the risk of developing cancer.
- Low risk: benign pancreas cysts with little or no chance of becoming cancerous such as pancreatitis related inflammatory fluid collections (sometimes called pseudocysts or false cysts), serous cystadenomas, simple cysts etc. These types of cysts need no intervention unless they cause symptoms.
- High risk: cancerous pancreas cysts or benign pancreas cysts that have the potential to progress over time to cancer. Most of these cysts are lined by a special layer of cells that secrete a type of mucus into the cysts. Taking all precancerous cysts into account, the overall risk of these developing into pancreatic cancer is approximately 5% over a 5 year period. This risk is modified higher or lower depending on multiple cyst features such as size, interval rate of growth, and involvement of the pancreatic duct.
Determination of whether a pancreas cyst is benign, precancerous or cancerous is the most important feature in the treatment of the cysts. A previous bout of a painful condition called pancreatitis (inflammation of the pancreas), usually indicates that the cyst may be inflammatory in nature.
While abdominal ultrasound, CT scan, and MRI scan can identify cysts, they cannot reliably distinguish benign cysts from precancerous or cancerous cysts. The test most commonly used for determination of cancer risk is called endoscopic ultrasound (EUS). EUS exam involves advancing an endoscope with an ultrasound transducer via the mouth and food pipe, into the stomach and upper small intestine (duodenum) bringing it close to the pancreas, liver, bile duct and gallbladder. EUS therefore allows accurate and detailed examination of the pancreas along with the ability to sample tissue as well as pancreas cyst fluid by passing special needles through the endoscope.
Fluid obtained from the pancreas cyst can be analyzed for cancerous cells (cytology), markers for inflammation, and for tumor markers. The risks of endoscopic ultrasound and fine needle aspiration are small and consist of a very small incidence of bleeding, infection, perforation of the stomach or intestine and pancreatitis (inflammation of the pancreas). Based on the information available after all tests, the cyst may be deemed benign, needing no follow up, reexamined by an imaging study after an appropriate interval or, surgery may be recommended.
FAQs
The vast majority of the pancreas cysts are benign when they are detected. Some cysts such as those that form after an attack of pancreatitis (pseudocysts), simple cysts and serous cystadenomas have no risk of turning into cancer. Other cysts that produce mucus (IPMNs or mucinous cystic neoplasms) are benign at time of diagnosis but have the potential to turn cancerous. Some cancers develop a liquified center as they grow larger and can mimic other types of cysts.
No. Cysts develop usually after a severe case of pancreatitis, particularly when there is necrosis of the pancreas gland due to pancreatitis.
Pancreatic cysts are usually diagnosed with imaging tests, such as CT scan or MRI, and a procedure called endoscopic ultrasound (EUS). EUS involves inserting a thin tube with an ultrasound probe into the digestive tract to get a close-up view of the pancreas. A biopsy, which involves removing a small sample of tissue for laboratory testing, may also be performed to confirm the diagnosis.
Treatment for pancreatic cysts depends on the type and size of the cyst, precancerous vs non-precancerous nature of the cysts as well as the presence of any cancerous cells. In some cases, a pancreatic cyst may be monitored with regular check-ups and imaging tests to see if it changes in size or appearance. Cysts as a result of pancreatitis may be drained during endoscopy if they cause symptoms or get infected. Surgery may be necessary to remove some cysts or affected part of the pancreas if it is large or contains cancerous cells.
There is no known way to prevent the development of pancreatic cysts. However, maintaining a healthy lifestyle, including not smoking, not abusing alcohol, and getting regular exercise, may reduce the risk of the disease.
The long-term outlook and prognosis for people with pancreatic cysts depends on the type and size of the cyst, as well as the presence of cancerous cells. If the cyst is small and does not contain cancerous cells, the prognosis is generally good. However, if the cyst is large or contains cancerous cells, the prognosis may be more serious.
A large proportion of cysts do not need any intervention other than periodic surveillance. If the pancreatic cyst is small and does not contain cancerous cells, it may be possible to cure the condition with endoscopic drainage or with surgery. However, if the cyst is large or contains cancerous cells, the chances of a cure may be lower. In these cases, treatment may be aimed at controlling the growth of cancerous cells.
In some cases, medications may be used to treat symptoms related to pancreatic cysts but in general, medications seldom have a role in treatment of pancreas cysts. For example, pancreatic enzyme supplements may be prescribed to help with digestion if the pancreas is not functioning properly.
It is generally recommended that people with pancreatic cysts maintain a healthy diet and exercise regularly to help manage the condition. However, specific lifestyle changes will depend on the individual’s specific situation and should be discussed with a healthcare provider.
It is possible for benign pancreatic cysts to recur after treatment, especially for the cysts seen after attacks of pancreatitis and precancerous cysts that produce mucus. Cancer containing cysts can spread and reoccur like any other cancers.